Moral judgements in
obsessive-compulsive disorder: a narrative mini-review
Mehrnaz
Hosseinzadeh, Elma Azhdehakosh and Adib Valibeygi *
Fasa Neuroscience Circle (FNC), Student Research
Committee, Fasa University of Medical Sciences, Fasa, Iran.
*
Correspondence: a.valibeygi@fums.ac.ir ; Tel.: +98-916-208-4125
Received: 8 October 2019; Accepted: 14 January 2020; Published: 13
February 2020
Edited by: King-Hwa Ling (Universiti Putra Malaysia, Malaysia/Harvard Medical
School, USA)
Reviewed by: Amedeo D'Angiulli (Carleton University, Canada);
Michael Wheaton (Columbia University, USA)
https://doi.org/10.31117/neuroscirn.v3i1.39
ABSTRACT: Obsessive-compulsive disorder (OCD) is a
prevalent mental disorder characterized by intrusive thoughts (obsessions) and
ensuing rituals (compulsions). Although OC patients exhibit various cognitive
and behavioral problems, rigid and hypersensitive moral judgments are known to
be one of the most striking problems in these patients. There is evidence
indicating that OC patients often tend to make deontological judgments in moral
dilemmas, significantly more than the healthy population. Therefore, numerous
studies are dedicated to understanding the underlying cognitive processes
responsible for such variation of moral judgments in OCD, which are reviewed
and discussed in the current paper. First, it is previously discussed that abnormal
moral judgments in OCD are due to executive dysfunctions. These dysfunctions
include impaired cognitive control resulting in the domination of strong,
uncontrolled emotional responses, impaired cognitive flexibility resulting in
the inability to switch between aspects of a scenario, and decreased capacity and
overload of working memory and its inability to resist the interfering
information. The dual-process theory also emphasizes and acknowledges the role
of executive functions in moral judgments. Second, it is thought that
disobeying moral norms results in the abnormal feeling of deontological guilt
in OC patients, to which these patients are highly sensitive. Feeling of guilt
is also thought to be correlated with OCD symptomatology. The third impairment
contributing to abnormal moral judgments in OCD is known to be the abnormal
feeling of disgust for moral violations and immoral unwanted intrusive
thoughts, which is regarded as one of the major causes of OCD symptoms.
Finally, the abnormal fear of responsibility and being criticized due to not
acting morally is regarded as one of the primary impairments contributing to
the abnormal moral judgments in OCD. In conclusion, this review sheds light on
the most striking cognitive and affective impairments contributing to abnormal
moral judgments in OCD.
Keywords: moral judgments; moral decision making; obsessive-compulsive
disorder; executive function; dual-process theory
©2020 by Hosseinzadeh et al. for use and distribution in accord with the
Creative Commons Attribution (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted
non-commercial use, distribution, and reproduction in any medium, provided the
original author and source are credited.
1.0 INTRODUCTION
Obsessive-compulsive disorder (OCD) is a common mental
disease which brings up the patient with unwanted intrusive thoughts. These
patients show a faulty appraisal of intruding thoughts (obsessions) that
results in compulsory rituals, such as washing or checking behaviors. Based on the Diagnostic and Statistical
Manual of Mental Disorders Fifth Edition (DSM-5), despite the overlapping
symptoms which OCD shares with depression and anxiety disorders, the distinct
features of OCD and related disorders make it a separate class of mental
disorders (American Psychiatric Association, 2013; Freeston
et al., 1996).
A well-functioning social group is dependent on the
appropriate judgment of the morality of behaviors to shape and ensure effective
interactions (Guglielmo, 2015). Numerous studies have investigated the quality of life and functional
impairments in OCD patients, indicating significant impairments in work, social,
and family life compared to healthy subjects. OCD patients especially have more
difficulty in social interactions including making new friends and being among a
group of strangers (Piacentini et al., 2003).
Human complex social systems rely on two important components: an integrative
system of rules, values and moral norms, and complex culture of practicing and
reinforcing these norms such as blame, inculpation, praise, and reconciliation (Voiklis
et al., 2017). The underlying social cognitive processes,
including the feeling of guilt, responsibility, disgust, reward learning,
valuation, empathy, caring and justice sensitivity, are fundamental for
sculpturing and maintaining this complex moral network. These processes are
found to be influenced by normal and pathological variations (Yoder
et al., 2018). Such variations may help explain observed
impairments in social interactions and the integration of psychopathically
affected individuals, particularly OCD patients.
Cognitive therapy is among the various treatments employed
for dealing with OCD. Adopting a suitable cognitive therapy procedure requires a
thorough understanding of cognitive and behavioral models. Various terms are
utilized for evaluating OC symptoms from the cognitive aspect, including
cognitive flexibility and working memory, which are reviewed and discussed in
the present study (Twohig
et al., 2006; Wilhelm et al., 2005).
One of the other discussed OCD topics is the potential
relevance between OCD and different types of emotions such as fear (Freeston
et al., 1996), anxiety (Obsessive
Compulsive Cognition Working Group, 1997), guilt (Melli
et al., 2016), and disgust (Stein
et al., 2010) which can influence moral judgments.
Generally, emotions are considered as internal intruding experiences that OCD
patients face. Anxiety and fear have been accounted for as the main emotions
involved in OCD (Chiang
& Purdon, 2019). Also, despite the increasing focus on guilt
and disgust among the recent studies, there are associations with OCD that
remain to uncover.
In the present review, we focus on the most striking
aspects of distorted cognitive processes in OC patients, which cause their abnormal
behavior in moral decision making. We searched PubMed and Google Scholar using
keywords: "obsessive-compulsive disorder," "moral judgments," "cognitive
flexibility," "working memory," "cognitive control," "responsibility," "disgust"
and "guilt." We had no
limitation of publication year in the literature search, but most of the papers
we considered were published in recent ten years. To improve the quality of the
review, we focused on the papers published by reputable international journals.
2.0 NEUROBIOLOGICAL BASIS OF OCD
Cortico-striato-thalamo-cortical (CSTC) circuit is
known to be one of the most important neural circuits involved in the neurobiology
of OCD. It is previously discussed that hyperactivity of this circuit,
including anterior cingulate
and orbitofrontal cortices (OFC), anterior thalamus, and striatum, is correlated with the
severity of OCD symptoms (Huey
et al., 2008; Pittenger et al., 2011). Also, decreased activity of Dorsolateral Prefrontal Cortex (DLPFC)
(which is known to be involved in working memory) is observed in OCD patients (Gaikwad,
2014; Saxena et al., 1998).
On the other hand, there is evidence of anatomical and
structural differences between the brains of patients with OCD and healthy
individuals, including increased caudate nucleus grey matter volume, bilateral
increase of putamen size, decrease of left anterior temporal lobe, and decrease
of right middle temporal gyrus volume in patients with OCD, as revealed by
Voxel-based morphometry studies (Besiroglu et al., 2011; Pittenger et al., 2011; Radua et al., 2010). It is noteworthy that increased caudate nucleus grey matter volume is
specific to OCD, but not other anxiety disorders (Pittenger et al., 2011).
Many studies are devoted to understanding the pathophysiological
basis of OCD. It is suggested that serotonin plays a considerable role in this
disorder and serotonergic circuits contribute to symptomatology of OCD. This is
why Selective Serotonin Reuptake Inhibitors (SSRIs) are widely used as a
treatment for OCD (Greenberg et al., 1997; Gaikwad, 2014; Pittenger et al., 2011).
However, the precise mechanism of their action remains unknown and requires
further investigations. Glutamate, an important neurotransmitter of the CSTC
circuit, has also drawn considerable attention in
terms of the role of its dysregulation in the pathogenesis of OCD. This
neurotransmitter is believed to serve a causal role in the onset of OCD (Pittenger et al., 2011).
It is discussed that OCD risk has a significant
association with polymorphism and mutations in some genes, including serotonin
transporter and glutamate related genes (Nestadt
et al., 2010). Additionally, it is shown that more than
half of the children with OCD have first degree relatives with this disorder (Gaikwad,
2014). Therefore, OCD is remarkably associated
with genetic factors, but still, further investigations are required to
identify the exact role of these mutations in prevalence and risk of OCD.
Regarding the neurobiological and pathophysiological
basis of OCD, several treatments are currently being used. Cognitive-behavioral
therapy and pharmacological therapy (e.g., administration of SSRIs) are the
commonly used treatments (Gaikwad,
2014; Pittenger et al., 2011). In severe refractory cases, neurosurgical interventions, including
Deep Brain Stimulation (DBS) (Greenberg et al., 2010) and
anterior cingulotomy (Gaikwad,
2014), would be beneficial.
3.0 MORAL JUDGMENTS IN
PATIENTS WITH OCD
There are several lines of evidence suggesting that OC
patients usually prefer deontological over utilitarian judgments while facing
moral dilemmas. In other words, they often focus on doing the right action (e.g.,
deontological view), rather than achieving the best outcomes. Conversely,
compared to OC patients, healthy individuals have more tendency to focus on
increasing overall happiness, decreasing overall suffering, and generally
achieving the best outcomes (e.g., utilitarian view) (Mancini
& Gangemi, 2015; Whitton et al., 2014). OC
patients adhere to moral norms more strictly, so they prefer to violate
altruistic and utilitarian principles, but not moral norms and rules (Mancini
& Gangemi, 2015; Whitton et al., 2014).
This moral rigidity and hypersensitive moral judgment, which is not seen in the
healthy population, reflects impaired cognitive processes in these patients.
Several investigations reported the underlying mechanisms and cognitive
processes responsible for such altered judgments, particularly in moral
dilemmas. There are neuroimaging studies that have
focused on the neural basis of distorted cognition in OCD patients. One of
these studies, recruiting fMRI, revealed increased activity of medial OFC, left
DLPFC and middle temporal gyrus in OCD patients (Harrison
et al., 2012). Nonetheless, there are yet
more brain regions believed to be associated with OCD pathogenesis that will be
reviewed in the next sections.
In the following section, we discuss various ethical
points of view and how they matter in understanding the mental processes of
moral decision making in OC patients.
4.0 UTILITARIAN AND DEONTOLOGICAL JUDGMENTS
There are two well-known and frequently used moral
dilemmas that can distinguish utilitarian and deontological thinking: the
footbridge dilemma and the switch dilemma. Footbridge dilemma is defined as
follows:
A trolley is heading toward five workmen
working on a track. If the trolley proceeds its way, it will run over these
five workmen and kill them. There is also a footbridge spanning the track with
a heavy person standing on it. The only way to rescue the five workmen on the track
is to push the heavy person off the footbridge. The trolley will run over and
kill him, but his heavy body will stop the trolley from proceeding its course,
and the five workmen will be saved.
This dilemma, which is a personal dilemma (Greene & Haidt, 2002),
asks an individual whether it is morally permissible to sacrifice one person
(by direct physical contact) to save five or not. Studies show that most people
tend to disagree (Greene
et al., 2001). It means that people will not allow
killing one person deliberately in this manner, even if this course of action
saves more lives. In other words, they mostly focus on the unpleasant action of
killing one person deliberately, rather than the overall beneficial outcomes.
This is known as the deontological point of view. Switch dilemma is defined as
follows:
A trolley is headed toward five workmen
working on a track. If the trolley proceeds its way, it will run over these
five workmen and kill them. But there is also an alternate track for the trolley,
on which one workman is working. The only way to save five workmen is hitting a
switch, which redirects the trolley toward only workman working on the
alternate track leading to his death but rescuing five other workmen.
This dilemma also asks an individual whether it is
morally permissible to sacrifice one person to save five but in a different
course of action than the footbridge dilemma. Previous studies have shown that
most people say yes (Greene
et al., 2001). Indeed, in the switch dilemma, which is
an impersonal dilemma (Greene
& Haidt, 2002), most people prefer to follow
utilitarianism principles, which means that they agree to save five at the
expense of one.
As explained above, both footbridge and switch dilemma
evaluate the moral permissibility of sacrificing one life to save five. While
most responses to the former are deontological, responses to the latter are
often utilitarian. This discrepancy is well explained by Waldmann and Dieterich
(Waldmann
& Dieterich, 2007). They used a scenario in which a bomb is
about to explode and kill 9
people. There were two
variants of this scenario. In the agent-intervention variant, individuals were
asked whether it is morally acceptable to throw a bomb in a place where one
person will be killed. In the patient-intervention variant, they were asked
whether it is morally acceptable to push a person on the bomb, leading to
his/her death but saving 9 people. Interestingly, they observed that most people
think it is morally acceptable to throw the bomb leading to kill one and save
9, while it is not morally acceptable to push a person on the bomb, leading to
the same result. They introduced the term "intervention myopia" for this
phenomenon. It means that when individuals focus on the locus of the
intervention, they tend to neglect the background happenings. When one is
focusing on throwing a person on the bomb, he/she will pay less attention to
the outcomes outside the attention focus (e.g., saving 9 people). Thus, this
action would be considered to be immoral. Conversely, in the agent-intervention
condition, the locus of attention is an object (bomb), not a person, leading
individuals to a different judgment (Nakamura,
2012; Waldmann & Dieterich, 2007).
This is also the case in the switch and footbridge
dilemmas. They both have the same outcome, but people prefer to take action in
the switch, but not footbridge dilemma, because in the former the locus of
attention and action is an agent (e.g., the switch), while in the latter the
locus of attention and action is a person (e.g., the victim). When focusing on
a victim, deontology is preferred, while when focusing on an object, utilitarianism
is preferred. What matters is the causal path and the locus of attention, while
the background happenings and outcomes are less considered (Nakamura,
2012; Waldmann & Dieterich, 2007). People also prefer indirect to direct harm. In the footbridge
dilemma, the harmful action is taking place directly and with physical contact
on a victim, without asking for consent, which violates moral norms (Nakamura,
2012; Waldmann & Dieterich, 2007). Emotional engagement is also another determinant factor accounting
for this difference. It is argued that pushing someone off the bridge leading
to her/his death evokes stronger emotional responses compared to just hitting a
switch (Greene
et al., 2001).
5.0 COGNITIVE IMPAIRMENTS CONTRIBUTING
TO ABNORMAL MORAL JUDGMENTS IN OC PATIENTS
In
order to investigate moral judgment as a complex form of decision-making, there
are lots of factors and components worth considering. In this study, we aim to establish
a synthetic model of cognitive and affective components contributing to moral
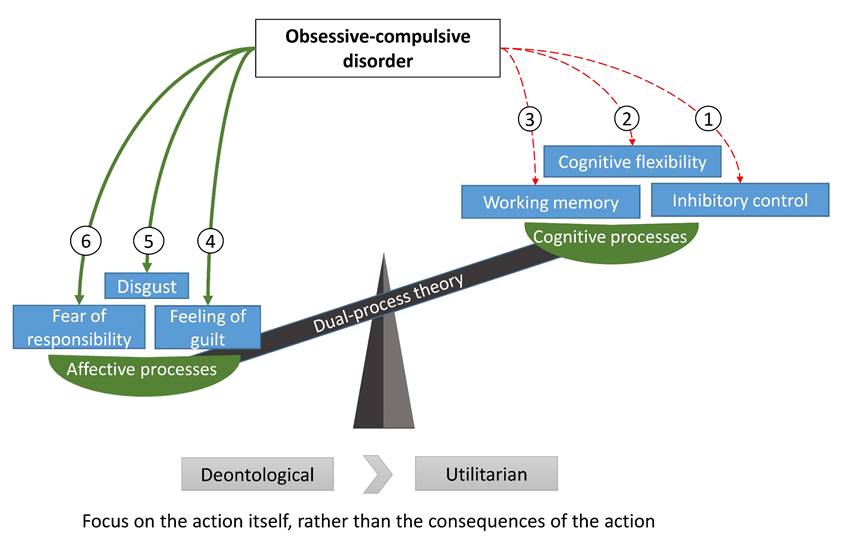
judgment in OCD patients (Figure 1).
5.1
Executive functions
Executive functions are among very important cognitive
processes that underlie selecting, modifying, and controlling behavior in
response to information and make the behavior more goal-directed. There are
several basic executive functions, including inhibitory cognitive control,
cognitive flexibility, and working memory. A handful of studies indicate
executive function impairment in neuropsychological disorders, including OCD (Baddeley,
1986; Baddeley & Hitch, 1974).
5.1.1 Inhibitory cognitive control and emotional
response
"Dual-process theory" suggests that two distinct
processes, controlled cognitive and automatic emotional processes, are involved
in moral judgments. According to this theory, automatic emotional responses to
dilemmas are associated with propensity for deontological options, while
controlled cognitive responses are associated with favoring utilitarian options
(Greene,
2009; Greene
et al., 2001; Lieberman et al., 2002).
Therefore, the domination of automatic emotional responses over-controlled
cognitive processes leads to favoring deontological options. Conversely, to
make a utilitarian judgment, emotions should be suppressed, and non-emotional
controlled cognitive processes should override automatic emotional responses. Therefore, impairments
in such inhibitory cognitive control result in a higher propensity for
deontological judgments. Since many of the moral scenarios presented to
subjects involve the death of one or more persons, such scenarios evoke strong
emotional responses in subjects that might interfere with non-emotional
cognitive processes. This point of view suggests that patients with OCD, who
are characterized by a higher tendency for choosing deontological options,
suffer from inflated emotional responses and deficits in inhibitory cognitive
control (Greene
et al., 2004; Whitton et al., 2014).
Also, Whitton et al. showed that OC patients are more rigid compared to
healthy individuals in impersonal dilemmas. This observation suggests more
emotion-driven judgments of OC patients in the context in which less emotional
response is expected (Whitton
et al., 2014).
A recent fMRI study in a resting state imaging has
demonstrated that OCD patients have relatively impaired functional connectivity
of the amygdala to some other brain regions, including insula. It is argued
that this impairment in emotion regulation systems contributes to abnormal
emotional processing in OCD patients (Picó‐Pérez et al., 2019).
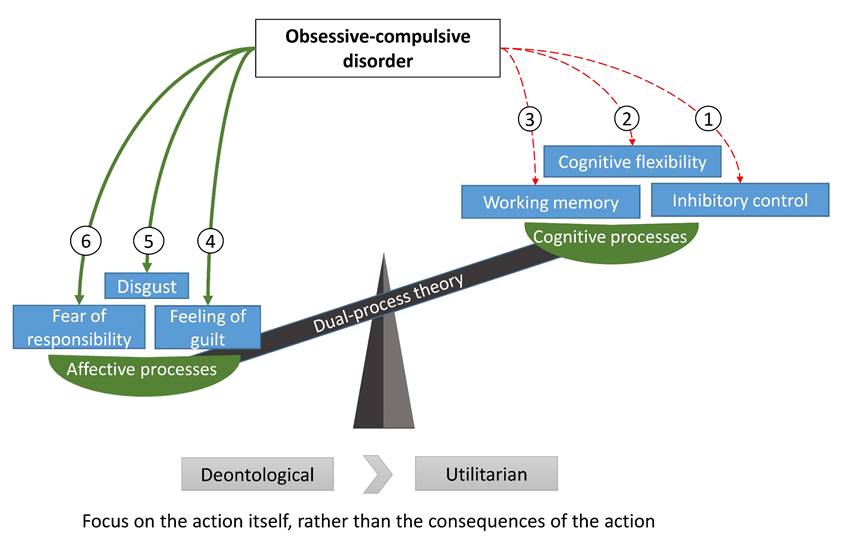
Figure 1. In
this synthetic model, the moral consequences of Obsessive-Compulsive Disorder
(OCD) are illustrated. 1. Impaired inhibitory control causes
uncontrolled emotional responses to overcome non-emotional processes, leading
to more propensity for deontology (Greene et al., 2008). 2.
Cognitive inflexibility makes it difficult for OC patients to divert their
center of attention from the action to its consequences. 3. Working
memory overload or dysfunction will lead to impulsive decision making. 4.
Patients with OCD have abnormal guilt processing. They have more sensitivity to
deontological guilt rather than utilitarian. 5. OCD patients have an
intense feeling of disgust for immorality, which makes them morally sensitive. 6.
OCD patients have an inflated sense of responsibility, which evokes fear
emotions and interferes with moral judgments. Taken all together, patients with
OCD have more propensity for deontological moral judgments in morally charged
situations.
5.1.2 Cognitive flexibility
Another significant executive function is cognitive
flexibility. One aspect of cognitive flexibility is the notion that in order to
make a utilitarian decision, one should switch her/his attention from the
action to the consequences of the action (Greene
et al., 2008; Whitton et al., 2014).
Switching focus between two different aspects of a scenario requires cognitive
flexibility, which is impaired in OC patients (Benzina
et al., 2019; Bigdeli et al., 2017; Şahin et al., 2018). Thus, they are incapable of switching their attention from the action
to the outcomes of the action. This inability leads to more than usual focus on
the action, which often has a negative affective load, and lower focus on the
outcomes. Therefore, reduced cognitive flexibility predicts a higher propensity
for deontological judgments (Whitton
et al., 2014). A recent neuroimaging study, recruiting resting-state
fMRI, has revealed that dysfunction of the connectivity between dorsal caudate
and salience network, including the anterior insula and dorsal ACC, is related to
impaired cognitive flexibility in OCD patients. However, whether this
functional impairment has a causal role in the development of OCD is yet to be
determined (Tomiyama
et al., 2019).
5.1.3 Working memory
Working memory is a key element in our daily lives in behaving,
thinking, reasoning, writing, and perceiving. It was first defined by Baddeley
as a cognitive process to temporarily store and manipulate information in order
to guide our behavior. In other words, it can be regarded as a temporary
workspace to store pieces of new information, reach long-term memory, mix and
manipulate information and process them to guide the behavior toward goals (Baddeley,
1986; Baddeley & Hitch, 1974).
Despite the lack of an integrative conclusion on
executive functions in OCD, there is a hypothetical abnormality in
cortico-basal-ganglia-thalamo-cortical loops (CBGTC loops) which involves
impaired recruitment of striatum. Unless the quite same performance in
different declarative and non-declarative memory tasks among OCD patients and
control subjects, neuroimaging studies reveal that OCD patients might use the
hippocampus which is involved in explicit learning to compensate deficit in
striatum-related or implicit memory (Maia
et al., 2008). More importantly, DLPFC, which is the
major brain region known to play a significant role in working memory, is found
to have altered activity in OCD. While some studies indicate decreased DLPFC
activity in OCD patients (Gaikwad,
2014), another finding does not agree (Harrison
et al., 2012). Therefore, more studies are required to
resolve or explain this contradiction. Thus, there is a subtle deficit in
complex non-verbal working memory tasks, as has been shown in several other studies
(Deckersbach et al., 2002; Jaafari et al., 2013; Purcell
et al., 1998). This explanation is consistent with
obsessions as hyperawareness of their actions and pathological overload of
working memory which may be feeble in resisting the interfering information, as
an important function of intact working memory (Barkley,
1997), and also compulsions which can be regarded
as striatum-dependent habit learning system overload and maladaptive use (Maia
et al., 2008). The concept of working memory impairment
in OCD was also tested in the neurocomputational approach, and Verduzco-Flores et
al. (2009) model
of working memory was promising in explaining the symptoms of OCD (Maia
& McClelland, 2012).
Previously discussed dual-process theory that was well
investigated in moral decision-making by Greene (Greene
et al., 2004) can be associated with moral decision
making in the way that personal dilemmas provoke a more emotional response, but
impersonal dilemmas acquire more deliberative reasoning and working memory.
This concept is consistent with studies that indicate people with high working
memory capacity are more rational (decision making based on situation and
consequences of action, known as utilitarian), better in overcoming salient
emotional response, and their reaction time is longer
than other groups, showing involved deliberative reasoning (Frankenstein, 2016; Moore et al., 2008). It is discussed that the relationship between moral reasoning ability
and working memory is more accurate than its relationship with age (Gibbs,
2019). The other important reason for how moral
development can be associated with working memory when an investigation is
performed on its bidirectional relation with social development which is the
fundamental component of moral learning and reinforcement (de
Wilde et al., 2016). A study by Hinson et al. on delay
discounting process showed that overloaded working memory due to either rich
information scenarios or reduced working memory capacity would lead to
impulsive decision making which in case of moral decision making would be the
deontological approach (Hinson
et al., 2003). In pursuit of developing a framework on
how human does moral judgments and particularly how this complex system
develops, Garrigan et al. developed the Social Information
Processing-Moral Decision-Making (SIP-MDM) framework, that was designed to
incorporate almost every related component of moral maturation and moral
decision making, working memory as one of the most important executive
functions which are shown to affect appropriate moral maturation. They regard
working memory as one of the critical components in moral development (Garrigan
et al., 2018).
5.2 Feeling of guilt
The feeling of guilt plays a critical role in moral
decision making. Deontological guilt points to the notion that one should not
violate the moral norms (Basile
& Mancini, 2011; Sunstein, 2005).
For example, in the case of the footbridge dilemma, the feeling of
deontological guilt does not permit to push the person off the bridge since
killing a person in violation of a moral norm, regardless of the consequences
and benefits of this action. It is also said that you do not have to play God:
"Who are you to decide who dies and who remains alive?" Therefore, refraining
from killing one person in order to adhere to moral norms and the rule of "Do
not play God" are considered as ways to avoid the feeling of deontological
guilt (Mancini
& Gangemi, 2015; Sunstein, 2005). On
the other hand, altruistic guilt points to the feeling of guilt, due to not
sharing others unpleasant fate, even if no moral rule is disobeyed (Basile
& Mancini, 2011). As previously discussed, OC patients are
more sensitive to deontological guilt than non-OCD individuals, so they decide
to avoid this feeling (e.g., they prefer inaction to action) (Mancini
& Gangemi, 2015).
To identify the underlying brain dysfunctions
accounting for abnormal guilt processing in OC patients, Basile et al. (2014) carried out an fMRI study. First, they found that OC patients are more
sensitive to deontological guilt, which is in line with previous findings.
Secondly, compared to the control group, patients with OCD showed decreased
activity in some brain regions, including ACC and insula, which are involved in
deontological guilt processing while they were presented with a guilt stimulus,
especially deontological. It is consistent with the neural efficiency
hypothesis, which explains that frequent activation of a brain network might
result in increased efficiency and therefore, decreased intensity of response
to stimuli. Similarly, in the case of OCD, related brain networks are
repeatedly activated due to guilt stimuli, resulting in the down-regulation of
their activity (Neubauer
& Fink, 2009).
Moreover, there is evidence supporting the association
between OCD symptoms and feelings of guilt. It was demonstrated that washing
behavior in OCD patients is associated with the sense of not only physical but
also mental cleansing. Reuven et al. (2014) carried out a study in which healthy individuals and OC patients were
asked to write about an immoral act they have had before. Then, some of them
were asked to wipe their hands. Surprisingly, it was observed that subjects,
especially OC patients, were less likely to help others in return of nothing
when they had wiped their hands. Likewise,
subjects who had not washed their hands showed more tendency to help. Reuven et al. also showed that hand
wiping, especially in OC patients, is associated with subsiding unpleasant
moral emotions (e.g., guilt, disgust, regret). This indicates that hand washing
relieves the feeling of guilt. Taken together, they concluded that OC patients
assign the physical cleansing to spiritual and mental cleansing and it relieves
their feeling of guilt. This effect, however, was not limited to washing
obsession patients (D'Olimpio & Mancini, 2014; Reuven et al., 2014). Besides, the induction of deontological guilt is accompanied by
increased washing and checking behaviors, which are known as typical OCD
symptoms, significantly more than altruistic guilt induction. These results
provide further evidence for the correlation between OCD symptomatology and the
feeling of deontological guilt (D'Olimpio & Mancini, 2014; Trafford
et al., 2018).
5.3 Feeling of disgust
Disgust is defined as the intense feeling
of revulsion or aversion for unpleasant stimuli. The correlation between OCD
and disgust is investigated and endorsed by several studies (Bhikram
et al., 2017; Inchausti et al., 2015). It is proposed that symptoms of OCD are
highly driven by the feeling of disgust to stimuli, suggesting a causal role
for disgust in OCD symptomatology. The feeling of disgust may be attributed to
contaminations (which account for washing rituals) or moral violations (which
account for moral rigidity) (Bhikram
et al., 2017; Olatunji et al., 2011). However, symmetry and checking obsessions are also
thought to be correlated with disgust (Bhikram
et al., 2017; Melli et al., 2015). In the case of morality, one's unwanted intrusive
thoughts, especially about sexual or religious transgressions, provoke morality
related feelings of disgust (Olatunji
et al., 2005; Vicario, 2013). Feeling
of guilt is also correlated with the level of disgust (D'Olimpio et al., 2013). A recent study by Robinson et al. (2019) found that
disgust sensitivity was associated with an increased propensity for
deontological judgments, which is mediated by the preference for respecting
orders (e.g., societal orders) (Robinson
et al., 2019). Taken together, an inflated
feeling of disgust is another mediator of sensitive moral judgment in OC
patients. Again, neuroimaging evidence supports the role of the dysregulation
of insula activity in OCD symptomatology, this time focusing on disgust
sensitivity (Viol
et al., 2019). On the other hand, Viol et
al. (2019) stated that disgust
sensitivity is related to the activation of DLPFC, caudate nucleus and visual association
cortex (VAC) (Rickelt
et al., 2019). More studies are required to
resolve or explain the inconsistency.
5.4 Fear of responsibility
Some obsessive behaviors in OCD are induced by an
inflated sense of responsibility and fear of being criticized and despised by
others due to not acting perfectly in a situation (Mancini
& Gangemi, 2011; Salkovskis et al., 2000). It has been shown that when the responsibility of action was
attributed to OC patients, they exhibited more obsessive behaviors, but when
the responsibility was averted to someone else, OC patients exhibited decreased
concerns and desires for their rituals (D'Olimpio & Mancini, 2014; Franklin
et al., 2009; Lopatka & Rachman, 1995). In
other words, OC patients, especially those with checking rituals, worried the
most about their responsibility and performance, rather than being altruistic
and worried about others' wellbeing. Likewise, when the responsibility of
action was assigned to healthy subjects, they will show OCD resembling
behaviors, compared to control subjects (Arntz
et al., 2007; Mancini & Gangemi, 2011).
Arntz et al. also showed a correlation between checking behaviors and
responsibility levels. Interestingly, they also suggested a causal role for the
responsibility beliefs in both the development and maintenance of checking
behaviors in OCD. However, this also applies to washing behaviors, aimed to
prevent guilt and responsibility due to contamination and resulted in illnesses
(D'Olimpio & Mancini, 2014).
Therefore, an inflated sense of responsibility can be considered as a target
for cognitive and behavioral therapy of OCD (Cosentino et al., 2012; Vos et al., 2012). However, D'Olimpio and Mancini claimed that the feeling of
responsibility could not explain the obsessive-compulsive rituals and behaviors
alone (D'Olimpio & Mancini, 2014). There
is not sufficient neuroimaging evidence of the association between fear of
responsibility and OCD incidence or symptomatology. Therefore, more
investigations are needed on this matter to gain more insight into the
pathophysiological and neural basis of abnormal fear of responsibility in OCD
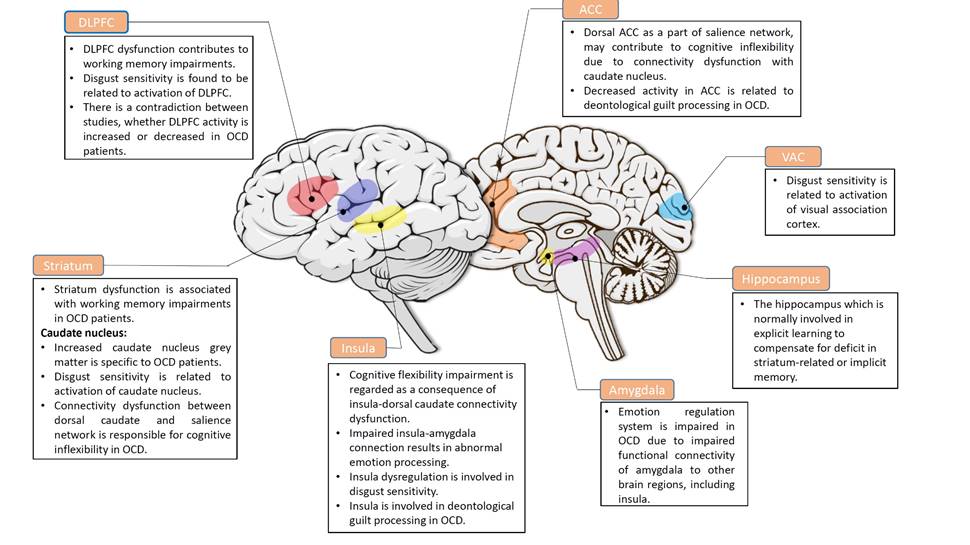
patients, in order to develop new potential treatments for the disease. Figure 2 represents a graphical summary of
the most striking neuroimaging findings regarding the brain regions involved in
the components discussed earlier.
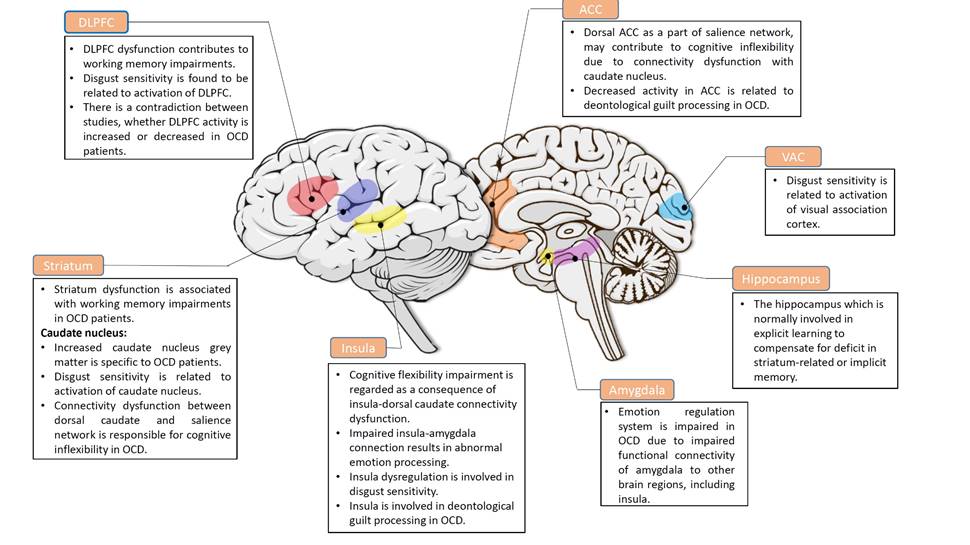
Figure 2. This figure shows a graphical abstract of the
important brain regions that are affected in pathophysiology and symptomatology
of OCD. The association between these abnormalities and OCD has to be studied
more. However, the precise neural basis of abnormal fear of responsibility
should be further investigated.
6.0 CONCLUSION
Numerous studies have demonstrated that deontology is the most
preferred type of moral thinking in individuals affected by OCD. In this review
study, we aimed to investigate some of the possible components of moral judgment
and decision making in light of available theories, especially the dual-process
theory, in OCD as one of the most common and debilitating mental disorders. Moral thinking is an essential aspect of
social living, as the social structure is maintained based on rules and norms
and a complex network for practicing and reinforcing these norms.
Executive dysfunctions, including impaired cognitive control,
cognitive inflexibility, and working memory dysfunction, are known to be among
the important problems in OC patients. It was discussed that OCD encompasses
deficits in inhibitory cognitive control. As a result of this deficit, patients
cannot maintain control over their emotional responses, especially in extreme
scenarios, involving the death of individuals. Such uncontrolled and inflated
emotional responses drive more rigid and deontological judgments in moral
scenarios. Almost in every decision-making process, deliberate reasoning is
preceded by intuitive thinking, as intuition needs less cognitive effort. Thus,
cognitive flexibility is required to divert the focus of attention from the
most emotional aspect of moral scenarios (the needed action) to the
consequences of actions that requires more cognitive effort. OCD encompasses a
deficit in cognitive flexibility, which can explain deontological preference.
Another executive function that is impaired in OCD is working memory, which is
argued to be abnormally overloaded by intrusive obsessive thoughts. It is shown
that overloaded working memory will result in more impulsive decision making.
Also, children with working memory problems have difficulty in learning and
practicing moral norms by participating in social activities; thus working
memory is regarded as one of the most important aspects of moral development.
The affective component of dual-process theory in moral decision
making is discussed here by investigating the abnormalities in the feeling of
guilt, feeling of disgust, and fear of responsibility in OCD. There is evidence
showing that OC patients are more susceptible to the guilt of deontology than
non-OC individuals, so they prefer decisions that get them rid of this guilty
feeling, for example, by choosing inaction over morally challenging actions.
Moreover, there is supporting evidence demonstrating the association between
feeling of guilt and induction of compulsive behaviors, suggesting a causal
role for abnormal guilt processing in OCD symptomatology. This indicates the
sensitivity to deontological guilt feelings in these patients. Also, the
inflated feeling of disgust, which is aversion for unpleasant stimuli such as
immorality, will induce more severe moral rigidity in these individuals.
Feeling of guilt is also known to be correlated with the feeling of disgust in these
patients. Moreover, fear of responsibility is also a crucial component in moral
thinking and behaving, which is argued to be inflated and significantly
associated with OCD symptoms.
Morality is a very crucial aspect in our daily lives and social
activities; thus abnormality in moral thinking will lead to issues in OCD
patients' lives, and having a clearer understanding of what exactly happens in
their moral thinking will help in enhancing their quality of life and social
functioning. Also, understanding the affected components in moral judgments and
developing richer cognitive models of the disease will lead to finding better
and more effective targets in cognitive therapy of OCD.
Our investigated components, including executive and affective
functions, lead to evidence of abnormalities in the way of explaining the
deontological preference in OC individuals, but further investigations on
finding a clearer picture of these components are needed to provide more
abundant evidence on their neuroscientific basis (e.g., fear of responsibility),
and the precise role of the neurotransmitters (e.g., glutamate) in
pathophysiology of the disorder, and effect of cultural and religious
differences (as most of the studies reviewed in this paper were from the United
States). Also, we believe that there would be far more components worth further
investigation and consideration, such as the role of stereotypes, feeling of
shame, development of a theory of mind, perfectionism, self-referential
thinking effect, culture, religion, and point of view on moral judgment.
Acknowledgments: We thank Fasa University of Medical Sciences for
providing financial support for this study and its support of the Fasa
Neuroscience Circle (FNC). We appreciate all FNC members, who have supported
and participated in the topic discussions on this project.
Author Contributions: All the authors contributed to searching, reading
papers, and writing the manuscript.
Conflicts of Interest: The authors declare no conflict of interest.
References
American
Psychiatric Association. (2013). Diagnostic and statistical manual of mental
disorders (DSM-5®): American Psychiatric Pub.
Arntz,
A., Voncken, M., & Goosen, A. C. (2007). Responsibility and obsessive-compulsive
disorder: An experimental test. Behaviour Research and Therapy, 45(3),
425-435. https://doi.org/10.1016/j.brat.2006.03.016
Baddeley,
A. D. (1986). Working memory Oxford. England: Oxford Uni.
Baddeley,
A. D., & Hitch, G. (1974). Working memory. In Psychology of learning and
motivation (Vol. 8, pp. 47-89): Elsevier.
Barkley,
R. A. (1997). Behavioral inhibition, sustained attention, and executive
functions: constructing a unifying theory of ADHD. Psychological Bulletin,
121(1), 65. Retrieved from https://doi.org/10.1037/0033-2909.121.1.65
Basile,
B., & Mancini, F. (2011). Eliciting guilty feelings: A preliminary study
differentiating deontological and altruistic guilt. Psychology, 2(2),
98-102. https://doi.org/10.4236/psych.2011.22016
Basile,
B., Mancini, F., Macaluso, E., Caltagirone, C., & Bozzali, M. (2014).
Abnormal processing of deontological guilt in obsessive-compulsive disorder. Brain
Structure and Function, 219(4), 1321-1331. https://doi.org/10.1007/s00429-013-0570-2
Benzina,
N., N'Diaye, K., Pelissolo, A., Mallet, L., & Burguière, E. (2019). A
cross-species assessment of cognitive flexibility in compulsive disorders. bioRxiv,
542100. https://doi.org/10.1101/542100
Besiroglu,
L., Sozen, M., Ozbebit, Ö., Avcu, S., Selvi, Y., Bora, A., Atli, A., Unal, O.,
& Bulut, M. (2011). The involvement of distinct neural systems in patients
with obsessive-compulsive disorder with autogenous and reactive obsessions. Acta
Psychiatrica Scandinavica, 124(2), 141-151. https://doi.org/10.1111/j.1600-0447.2011.01726.x
Bhikram,
T., Abi-Jaoude, E., & Sandor, P. (2017). OCD: obsessive-compulsive...
disgust? The role of disgust in obsessive-compulsive disorder. Journal of Psychiatry
& Neuroscience: JPN, 42(5), 300-306. https://dx.doi.org/10.1503%2Fjpn.160079
Bigdeli,
I., Badin, M., & Sabahi, P. (2017). The comparison of Cognitive
Flexibility, theory of mind and working memory in students with symptoms of
obsessive-compulsive disorder and normal group. Advances in Cognitive Sciences, 18(4), 24-37.
Chiang,
B., & Purdon, C. (2019). Have I done enough to avoid blame? Fear of guilt
evokes OCD-like indecisiveness. Journal of Obsessive-Compulsive and Related Disorders,
20, 13-20. https://doi.org/10.1016/j.jocrd.2018.02.001
Cosentino,
T., D'Olimpio, F., Perdighe, C., Romano, G., Saliani, A., & Mancini, F.
(2012). Acceptance of being guilty in the treatment of obsessive-compulsive
disorder. Psicoterapia Cognitiva e Comportamentale, 18(3), 39-56.
D'Olimpio,
F., Cosentino, T., Basile, B., Tenore, K., Gragnani, A., & Mancini, F.
(2013). Obsessive-compulsive disorder and propensity to guilt feelings and to
disgust. Clinical Neuropsychiatry, 10(3 Suppl.1), 20-29.
D'Olimpio,
F., & Mancini, F. (2014). Role of deontological guilt in
obsessive-compulsive disorder-like checking and washing behaviors. Clinical
Psychological Science, 2(6), 727-739. https://doi.org/10.1177%2F2167702614529549
de
Wilde, A., Koot, H. M., & van Lier, P. A. C. (2016). Developmental links
between children's working memory and their social relations with teachers and
peers in the early school years. Journal of Abnormal Child Psychology, 44(1),
19-30. https://doi.org/10.1007/s10802-015-0053-4
Deckersbach,
T., Savage, C. R., Curran, T., Bohne, A., Wilhelm, S., Baer, L., Jenike, M. A.,
&. Rauch, S. L. (2002). A study of parallel implicit and explicit
information processing in patients with obsessive-compulsive disorder. American
Journal of Psychiatry, 159(10), 1780-1782. https://doi.org/10.1176/appi.ajp.159.10.1780
Frankenstein,
A. (2016). To Kill or Not to Kill: Exploring the Roles of Empathy and Working
Memory in Moral Decision Making. UNF
Graduate Theses and Dissertations. 625. https://digitalcommons.unf.edu/etd/625
Franklin,
S. A., McNally, R. J., & Riemann, B. C. (2009). Moral reasoning in
obsessive-compulsive disorder. Journal of Anxiety Disorders, 23(5),
575-577. https://doi.org/10.1016/j.janxdis.2008.11.005
Freeston,
M. H., Rhéaume, J., & Ladouceur, R. (1996). Correcting faulty appraisals of
obsessional thoughts. Behaviour Research and Therapy, 34(5-6), 433-446. https://doi.org/10.1016/0005-7967(95)00076-3
Gaikwad,
U. (2014). Pathophysiology of obsessive-compulsive disorder: affected brain
regions and challenge towards discovery of novel drug treatment. In Obsessive-Compulsive
Disorder-The Old and the New Problems: IntechOpen. https://doi.org/10.5772/56999
Garrigan,
B., Adlam, A. L., & Langdon, P. E. (2018). Moral decision-making and moral
development: Toward an integrative framework. Developmental Review, 49,
80-100. https://doi.org/10.1016/j.dr.2018.06.001
Gibbs,
J. C. (2019). Moral development and reality: Beyond the theories of
Kohlberg, Hoffman, and Haidt: Oxford University Press.
Greenberg,
B. D., Altemus, M., & Murphy, D. L. (1997). The role of neurotransmitters
and neurohormones in obsessive-compulsive disorder. International Review of
Psychiatry, 9(1), 31-44. https://doi.org/10.1080/09540269775574
Greenberg, B. D.,
Rauch, S. L., & Haber, S. N. (2010). Invasive circuitry-based
neurotherapeutics: stereotactic ablation and deep brain stimulation for OCD. Neuropsychopharmacology,
35(1), 317. https://doi.org/10.1038/npp.2009.128
Greene,
J., & Haidt, J. (2002). How (and where) does moral judgment work? Trends
in Cognitive Sciences, 6(12), 517-523. https://doi.org/10.1016/S1364-6613(02)02011-9
Greene,
J. D. (2009). Dual-process morality and the personal/impersonal distinction: A
reply to McGuire, Langdon, Coltheart, and Mackenzie. Journal of Experimental
Social Psychology, 45(3), 581-584. https://doi.org/10.1016/j.jesp.2009.01.003
Greene,
J. D., Morelli, S. A., Lowenberg, K., Nystrom, L. E., & Cohen, J. D.
(2008). Cognitive load selectively interferes with utilitarian moral judgment. Cognition,
107(3), 1144-1154. https://doi.org/10.1016/j.cognition.2007.11.004
Greene,
J. D., Nystrom, L. E., Engell, A. D., Darley, J. M., & Cohen, J. D. (2004).
The neural bases of cognitive conflict and control in moral judgment. Neuron,
44(2), 389-400. https://doi.org/10.1016/j.neuron.2004.09.027
Greene,
J. D., Sommerville, R. B., Nystrom, L. E., Darley, J. M., & Cohen, J. D.
(2001). An fMRI investigation of emotional engagement in moral judgment. Science,
293(5537), 2105-2108. https://doi.org/10.1126/science.1062872
Guglielmo S. (2015). Moral judgment as information processing: an
integrative review. Frontiers in Psychology, 6, 1637.
doi:10.3389/fpsyg.2015.01637
Harrison,
B. J., Pujol, J., Soriano-Mas, C., Hernández-Ribas, R., López-Solà, M., Ortiz,
H., Alonso, P., Deus, J., Menchon, J. M., Real, E., Segalàs, C.,
Contreras-Rodríguez, O., Blanco-Hinojo, L., & Cardoner N. (2012). Neural
correlates of moral sensitivity in obsessive-compulsive disorder. Archives
of General Psychiatry, 69(7), 741-749. https://doi.org/10.1001/archgenpsychiatry.2011.2165
Hinson, J. M., Jameson,
T. L., & Whitney, P. (2003). Impulsive decision making and working memory.
Journal of Experimental
Psychology: Learning, Memory, and Cognition, 29(2), 298-306.
https://doi.org/10.1037/0278-7393.29.2.298
Huey,
E. D., Zahn, R., Krueger, F., Moll, J., Kapogiannis, D., Wassermann, E. M.,
& Grafman, J. (2008). A psychological and neuroanatomical model of
obsessive-compulsive disorder. The Journal of Neuropsychiatry and Clinical Neurosciences,
20(4), 390-408. https://doi.org/10.1176/jnp.2008.20.4.390
Inchausti,
F., Delgado, A. R., & Prieto, G. (2015). Obsessive-compulsive disorder and
its relationship with disgust vulnerability and conscientiousness. Psicothema,
27(3), 254-260. https://doi.org/10.7334/psicothema2015.7
Jaafari,
N., Frasca, M., Rigalleau, F., Rachid, F., Gil, R., Olié, J.-P., Guehl, D.,
Burbaud, P., Aouizerate, B., Rotgé, J. Y., & Vibert, N. (2013). Forgetting
what you have checked: A link between working memory impairment and checking
behaviors in obsessive-compulsive disorder. European Psychiatry, 28(2),
87-93. https://doi.org/10.1016/j.eurpsy.2011.07.001
Lieberman,
M. D., Gaunt, R., Gilbert, D. T., & Trope, Y. (2002). Reflexion and
reflection: A social cognitive neuroscience approach to attributional
inference. Advances in Experimental Social Psychology, 34,
199-249. https://doi.org/10.1016/S0065-2601(02)80006-5
Lopatka,
C., & Rachman, S. (1995). Perceived responsibility and compulsive checking:
An experimental analysis. Behaviour Research and Therapy, 33(6),
673-684. https://doi.org/10.1016/0005-7967(94)00089-3
Maia,
T. V., Cooney, R. E., & Peterson, B. S. (2008). The neural bases of
obsessive-compulsive disorder in children and adults. Development and Psychopathology,
20(4), 1251-1283. https://doi.org/10.1017/S0954579408000606
Maia,
T. V., & McClelland, J. L. (2012). A neurocomputational approach to
obsessive-compulsive disorder. Trends in Cognitive Sciences, 16(1),
14-15. https://doi.org/10.1016/j.tics.2011.11.011
Mancini,
F., & Gangemi, A. (2011). Fear of deontological guilt and fear of
contamination in obsessive-compulsive disorder. Psicoterapia Cognitiva e
Comportamentale, 17(3), 395-404.
Mancini,
F., & Gangemi, A. (2015). Deontological guilt and obsessive compulsive
disorder. Journal of Behavior Therapy and Experimental Psychiatry, 49,
157-163. https://doi.org/10.1016/j.jbtep.2015.05.003
Melli,
G., Aardema, F., & Moulding, R. (2016). Fear of self and unacceptable
thoughts in obsessive-compulsive disorder. Clinical Psychology and Psychotherapy,
23(3), 226-235. https://doi.org/10.1002/cpp.1950
Melli,
G., Chiorri, C., Carraresi, C., Stopani, E., & Bulli, F. (2015). The role
of disgust propensity and trait guilt in OCD symptoms: A multiple regression
model in a clinical sample. Journal of Obsessive-Compulsive and Related Disorders,
5, 43-48. https://doi.org/10.1016/j.jocrd.2015.01.007
Moore,
A. B., Clark, B. A., & Kane, M. J. (2008). Who shalt not kill? Individual
differences in working memory capacity, executive control, and moral judgment.
Psychological Science, 19(6), 549-557. https://doi.org/10.1111/j.1467-9280.2008.02122.x
Nakamura,
K. (2012). The Footbridge Dilemma Reflects More Utilitarian Thinking Than
The Trolley Dilemma: Effect Of Number Of Victims In Moral Dilemmas. Paper
presented at the Proceedings of the Annual Meeting of the Cognitive Science
Society. 803-808.
Nestadt,
G., Grados, M., & Samuels, J. F. (2010). Genetics of obsessive-compulsive
disorder. The Psychiatric Clinics of North America, 33(1), 141-158. https://doi.org/10.1016/j.psc.2009.11.001
Neubauer,
A. C., & Fink, A. (2009). Intelligence and neural efficiency. Neuroscience
& Biobehavioral Reviews, 33(7), 1004-1023. https://doi.org/10.1016/j.neubiorev.2009.04.001
Obsessive
Compulsive Cognition Working Group. (1997). Cognitive assessment of
obsessive-compulsive disorder. Behaviour Research and Therapy, 35(7),
667-681. https://doi.org/10.1016/S0005-7967(97)00017-X
Olatunji, B. O.,
Ebesutani, C., David, B., Fan, Q., & McGrath, P. B. (2011). Disgust
proneness and obsessive-compulsive symptoms in a clinical sample: Structural
differentiation from negative affect. Journal of Anxiety Disorders, 25(7),
932-938. https://doi.org/10.1016/j.janxdis.2011.05.006
Olatunji,
B. O., Tolin, D. F., Huppert, J. D., & Lohr, J. M. (2005). The relation
between fearfulness, disgust sensitivity and religious obsessions in a
non-clinical sample. Personality and Individual Differences, 38(4),
891-902. https://doi.org/10.1016/j.paid.2004.06.012
Piacentini,
J., Bergman, R. L., Keller, M., McCracken, J. (2003). Functional impairment in
children and adolescents with obsessive-compulsive disorder. Journal of
Child and Adolescent Psychopharmacology, 13(Supplement 1), S61-69. https://doi.org/10.1089/104454603322126359
Picó‐Pérez,
M., Ipser, J., Taylor, P., Alonso, P., López-Solà, C., Real, E., Segalàs,
C., Roos, A., Menchón, J. M., Stein, D. J., & Soriano-Mas, C. (2019).
Intrinsic functional and structural connectivity of emotion regulation networks
in obsessive‐compulsive disorder. Depression and Anxiety, 36(2),
110-120. https://doi.org/10.1002/da.22845
Pittenger,
C., Bloch, M. H., & Williams, K. (2011). Glutamate abnormalities in
obsessive compulsive disorder: neurobiology, pathophysiology, and treatment. Pharmacology
& Therapeutics, 132(3), 314-332. https://doi.org/10.1016/j.pharmthera.2011.09.006
Purcell,
R., Maruff, P., Kyrios, M., & Pantelis, C. (1998). Cognitive deficits in
obsessive-compulsive disorder on tests of frontal-striatal function. Biological
Psychiatry, 43(5), 348-357. https://doi.org/10.1016/S0006-3223(97)00201-1
Radua,
J., van den Heuvel, O. A., Surguladze, S., & Mataix-Cols, D. (2010).
Meta-analytical comparison of voxel-based morphometry studies in
obsessive-compulsive disorder vs other anxiety disorders. Archives of General
Psychiatry, 67(7), 701-711. https://doi.org/10.1001/archgenpsychiatry.2010.70
Reuven,
O., Liberman, N., & Dar, R. (2014). The effect of physical cleaning on
threatened morality in individuals with obsessive-compulsive disorder. Clinical
Psychological Science, 2(2), 224-229. https://doi.org/10.1177%2F2167702613485565
Rickelt,
J., de Wit, S. J., van der Werf, Y. D., Schruers, K. R., Marcelis, M., de
Vries, F. E., & van den Heuvel, O. A. (2019). Emotional processing and
disgust sensitivity in OCD patients with and without contamination-type
obsessive-compulsive symptoms-An fMRI study. Journal of Obsessive-Compulsive
and Related Disorders, 22, 100443. https://doi.org/10.1016/j.jocrd.2019.100443
Robinson,
J. S., Xu, X., & Plaks, J. E. (2019). Disgust and deontology: Trait
sensitivity to contamination promotes a preference for order, hierarchy, and
rule-based moral judgment. Social Psychological and Personality Science, 10(1),
3-14. https://doi.org/10.1177%2F1948550617732609
Şahin,
H., KÖşger, F., EşSizoğlu, A., & Aksaray, G. (2018). The
Relationship Between Obsessive Belief Level and Cognitive Flexibility in
Patients with Obsessive Compulsive Disorder. Archives of Neuropsychiatry, 55(4),
376-379. https://dx.doi.org/10.5152%2Fnpa.2017.21648
Salkovskis,
P. M., Wroe, A., Gledhill, A., Morrison, N., Forrester, E., Richards, C., Reynolds,
M., & Thorpe, S. (2000). Responsibility attitudes and interpretations are
characteristic of obsessive compulsive disorder. Behaviour Research and Therapy,
38(4), 347-372. https://doi.org/10.1016/S0005-7967(99)00071-6
Saxena,
S., Brody, A. L., Schwartz, J. M., & Baxter, L. R. (1998). Neuroimaging and
frontal-subcortical circuitry in obsessive-compulsive disorder. The British
Journal of Psychiatry, 173(S35), 26-37.
Stein,
D. J., Fineberg, N. A., Bienvenu, O. J., Denys, D., Lochner, C., Nestadt, G., Leckman,
J. F., Rauch, S. L., & Phillips, K. A. (2010). Should OCD be classified as
an anxiety disorder in DSM‐V? Depression and Anxiety, 27(6),
495-506. https://doi.org/10.1002/da.20699
Sunstein,
C. R. (2005). Moral heuristics. Behavioral and Brain Sciences, 28(4),
531-542. https://doi.org/10.1017/S0140525X05000099
Tomiyama,
H., Nakao, T., Murayama, K., Nemoto, K., Ikari, K., Yamada, S., Kuwano, M.,
Hasuzawa, S., Togao, O., Hiwatashi, A., & Kanba S. (2019). Dysfunction
between dorsal caudate and salience network associated with impaired cognitive
flexibility in obsessive-compulsive disorder: A resting-state fMRI study. NeuroImage:
Clinical, 24, 102004. https://doi.org/10.1016/j.nicl.2019.102004
Trafford,
A. A., Wroe, A. L., Brown, G., & Luzon, O. (2018). What you see is what you
do: Imagery and the moral judgements of individuals with OCD. Journal of Obsessive-Compulsive
and Related Disorders, 16, 50-55. https://doi.org/10.1016/j.jocrd.2017.12.002
Twohig,
M. P., Hayes, S. C., & Masuda, A. (2006). Increasing willingness to
experience obsessions: Acceptance and commitment therapy as a treatment for
obsessive-compulsive disorder. Behavior Therapy, 37(1), 3-13. https://doi.org/10.1016/j.beth.2005.02.001
Verduzco-Flores, S., Bodner, M., Ermentrout, B., Fuster, J. M., &
Zhou, Y. (2009). Working memory cells' behavior may be explained by
cross-regional networks with synaptic facilitation. PloS one, 4(8), e6399.
https://doi.org/10.1371/journal.pone.0006399
Vicario,
C. M. (2013). Morality and disgust: insights from obsessive compulsive
disorder. Frontiers in Psychiatry, 3, 113. https://doi.org/10.3389/fpsyt.2012.00113
Viol,
K., Aas, B., Kastinger, A., Kronbichler, M., SchÖller, H. J., Reiter, E.-M., Said-Yürekli,
S., Kronbichler, L., Kravanja-Spannberger, B., StÖger-Schmidinger, B., Aichhorn,
W., & Schiepek, G. K. (2019). Erroneously disgusted: fMRI study supports
disgust-related neural reuse in Obsessive-Compulsive Disorder (OCD). Frontiers
in Behavioral Neuroscience, 13, 81. https://dx.doi.org/10.3389%2Ffnbeh.2019.00081
Voiklis,
J., & Malle, B. F. (2018). Moral cognition and its basis in social
cognition and social regulation. In K. Gray & J. Graham (Eds.), Atlas of
moral psychology (p. 108-120). The Guilford Press.
Vos,
S. P., Huibers, M. J., & Arntz, A. (2012). Experimental investigation of
targeting responsibility versus danger in cognitive therapy of
obsessive‐compulsive disorder. Depression and Anxiety, 29(7),
629-637. https://doi.org/10.1002/da.21915
Waldmann,
M. R., & Dieterich, J. H. (2007). Throwing a bomb on a person versus
throwing a person on a bomb: Intervention myopia in moral intuitions. Psychological
Science, 18(3), 247-253. https://doi.org/10.1111%2Fj.1467-9280.2007.01884.x
Whitton,
A. E., Henry, J. D., & Grisham, J. R. (2014). Moral rigidity in
obsessive-compulsive disorder: Do abnormalities in inhibitory control,
cognitive flexibility and disgust play a role? Journal of Behavior Therapy
and Experimental Psychiatry, 45(1), 152-159. https://doi.org/10.1016/j.jbtep.2013.10.001
Wilhelm,
S., Steketee, G., Reilly-Harrington, N. A., & Deckersbach, T., Buhlmann,
U., & Baer, L. (2005). Effectiveness of cognitive therapy for
obsessive-compulsive disorder: An open trial. Journal of Cognitive
Psychotherapy, 19(2), 173-179. https://psycnet.apa.org/doi/10.1891/jcop.19.2.173.66792
Yoder,
K. J., Decety, J. (2018). The neuroscience of morality and social
decision-making. Psychology, Crime & Law, 24(3), 279-295. https://doi.org/10.1080/1068316X.2017.1414817
![]()