References
1.
Diagnostic and
Statistical Manual of Mental Disorders (DSM-5®). Fifth edition. American
Psychiatric Publishing, Incorporated; 2013. pp. 991, ISBN:978-0-89042-554-1.
2.
Vos T, Allen C, Arora M, Barber
RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence,
prevalence, and years lived with disability for 310 diseases and injuries,
1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet.
2016;388(10053):1545-1602. https://doi.org/10.1016/S0140-6736(16)31678-6
3.
Kessler RC, Merikangas KR, Wang
PS. Prevalence, comorbidity, and service utilization for mood disorders in the
United States at the beginning of the twenty-first century. Annu Rev Clin
Psychol. 2007;3:137-158. https://doi.org/10.1146/annurev.clinpsy.3.022806.091444
4.
Nazree NE, Loke AC, Zainal NZ,
& Mohamed Z. Lack of association between TPH2 gene polymorphisms with major
depressive disorder in multiethnic Malaysian population. Asia Pac Psychiatry.
2015;7(1):72-77. https://doi.org/10.1111/appy.12118
5.
Lian LH, Loke AC, Zainal NZ,
Mohamed Z. Association study of the tryptophan hydroxylase 1 gene with major
depressive disorder in three ethnic groups of the Malaysian population. Asian
Biomed. 2013;7(1):105-112. https://doi.org/10.5372/1905-7415.0701.156
6.
Aldoghachi AF, Tor YS, Redzun SZ,
Lokman KA, Razaq NA, Shahbudin AF, et al. Screening of brain-derived
neurotrophic factor (BDNF) single nucleotide polymorphisms and plasma BDNF
levels among Malaysian major depressive disorder patients. PloS One.
2019;14(1):e0211241. https://doi.org/10.1371/journal.pone.0211241
7.
Tiong CP, Loke AC, Mohamed Z,
Zainal NZ. Serotonin transporter gene polymorphism is associated with antidepressant
response to escitalopram in multiethnic Malaysians with major depressive disorder:
a preliminary study. Malay J Psychiatr. 2013;22(2):59-71.
8.
Bonhomme N, Esposito E.
Involvement of serotonin and dopamine in the mechanism of action of novel
antidepressant drugs: a review. J Clin Psychopharmacol. 1998;18(6):447-454.
https://www.ncbi.nlm.nih.gov/pubmed/9864076
9.
Davis C, Loxton NJ, Levitan RD,
Kaplan AS, Carter JC, Kennedy JL. 'Food addiction' and its association with a
dopaminergic multilocus genetic profile. Physiol Behav. 2013;118:63-69. https://doi.org/10.1016/j.physbeh.2013.05.014
10.
Gatt JM, Burton KL, Williams LM,
Schofield PR. Specific and common genes implicated across major mental
disorders: a review of meta-analysis studies. J Psychiatr Res. 2015;60:1-13.
https://doi.org/10.1016/j.jpsychires.2014.09.014
11.
Huang CC, Lu RB, Shih MC, Yen CH,
Huang SY. Association study of the dopamine transporter gene with personality
traits and major depressive disorder in the Han Chinese population. Pharmacogenet
Genom. 2011;21(2):94-97. https://doi.org/10.1097/FPC.0b013e3283424d94
12.
Joyce PR, Stephenson J, Kennedy
MA, Mulder RT, McHugh PC. The presence of both serotonin 1A receptor (HTR1A)
and dopamine transporter (DAT1) gene variants increase the risk of borderline
personality disorder. Front Genet. 2014;4:313. https://doi.org/10.3389/fgene.2013.00313
13.
Willner P. The mesolimbic dopamine
system as a target for rapid antidepressant action. Int Clin Psychopharmacol.
1997; 12(Suppl 3):S7-S14. http://dx.doi.org/10.1097/00004850-199707003-00002
14.
Dunlop BW, Nemeroff CB. The role
of dopamine in the pathophysiology of depression. Arch Gen Psychiatry.
2007;64(3):327-337. https://doi.org/10.1001/archpsyc.64.3.327
15.
Hall H, Halldin C, Guilloteau D,
Chalon S, Emond P, Besnard JC, et al. Visualization of the dopamine transporter
in the human brain postmortem with the new selective ligand [125I]PE2I. Neuroimage.
1999;9(1):108-116. https://doi.org/10.1006/nimg.1998.0366
16.
Giros BR, el Mestikawy
SA, Godinot NA, Zheng KE, Han HO, Yang-Feng TE, et al. Cloning, pharmacological
characterization, and chromosome assignment of the human dopamine transporter. Mol
Pharmacol. 1992;42(3):383-390. https://www.ncbi.nlm.nih.gov/pubmed/1406597
17.
Vandenbergh DJ, Persico
AM, Hawkins AL, Griffin CA, Li X, Jabs EW, et al. Human dopamine transporter
gene (DAT1) maps to chromosome 5p15.3 and displays a VNTR. Genomics.
1992;14(4):1104-1106. https://doi.org/10.1016/S0888-7543(05)80138-7
18.
Ciliax BJ, Heilman C,
Demchyshyn LL, Pristupa ZB, Ince E, Hersch SM, et al. The dopamine transporter:
immunochemical characterization and localization in brain. J Neurosci.
1995;15(3):1714-1723. https://doi.org/10.1523/JNEUROSCI.15-03-01714.1995
19.
Haeffel GJ, Getchell M,
Koposov RA, Yrigollen CM, De Young CG, Klinteberg BA, et al. Association
between polymorphisms in the dopamine transporter gene and depression: evidence
for a gene-environment interaction in a sample of juvenile detainees. Psychol
Sci. 2008;19(1):62-69. https://doi.org/10.1111/j.1467-9280.2008.02047.x
20.
Pattarachotanant N,
Sritharathikhun T, Suttirat S, Tencomnao T. Association of C/T polymorphism in
intron 14 of the dopamine transporter gene (rs40184) with major depression in a
northeastern Thai population. Genet Mol Res. 2010;9(1):565-572. https://doi.org/10.4238/vol9-1gmr757
21.
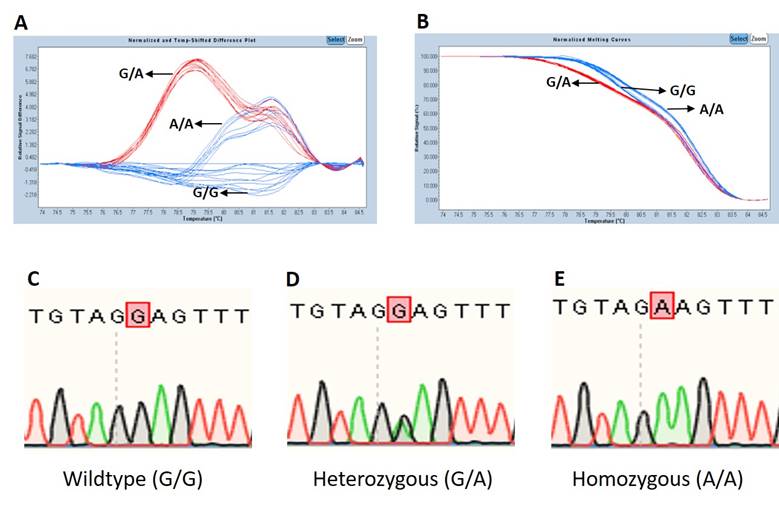
Faris A, Yusof HH,
Abidin SZ, Habib O, Cheah PS, Stanslas J, et al. Development and validation of
high resolution melting assays for high-throughput screening of BDNF rs6265 and
DAT1 rs40184. Malay J Med Health Sci. 2018;14(SP1):64-71.
22.
Der-Avakian A, Markou
A. The neurobiology of anhedonia and other reward-related deficits. Trends
Neurosci. 2012;35(1):68-77. https://doi.org/10.1016/j.tins.2011.11.005
23.
Donald SR, Robinson MD.
The role of dopamine and norepinephrine in depression. Prim Psychiatry.
2007;14(5):21-23.
24.
Mick E, Kim JW,
Biederman J, Wozniak J, Wilens T, Spencer T, et al. Family based association
study of pediatric bipolar disorder and the dopamine transporter gene (SLC6A3).
Am J Med Genet. 2008;147B(7):1182-1185. https://doi.org/10.1002/ajmg.b.30745
25.
Zhou K, Chen W,
Buitelaar J, Banaschewski T, Oades RD, Franke B, et al. Genetic heterogeneity
in ADHD: DAT1 gene only affects probands without CD. Am J Med Genet.
2008;147B(8):1481-1487. https://doi.org/10.1002/ajmg.b.30644
26.
Hardy GH. Mendelian
proportions in a mixed population. Science. 1908;28(706):49-50. https://doi.org/10.1126/science.28.706.49
27.
Garnier-Géré P,
Chikhi L. Population Subdivision, Hardy-Weinberg Equilibrium and the Wahlund
Effect. In eLS, John Wiley & Sons, Ltd (Ed.). 2013. https://doi.org/10.1002/9780470015902.a0005446.pub3
28.
Otte C, Gold SM,
Penninx BW, Pariante CM, Etkin A, Fava M, et al. Major depressive disorder. Nat
Rev Dis Primers. 2016;2:16065. https://doi.org/10.1038/nrdp.2016.65
29.
Popa TA, Ladea M.
Nutrition and depression at the forefront of progress. J Med Life.
2012;5(4):414-419.
30.
Sarris J, O'Neil A,
Coulson CE, Schweitzer I, Berk M. Lifestyle medicine for depression. BMC
Psychiatry. 2014;14(1):107. https://doi.org/10.1186/1471-244X-14-107
31.
Levinson DF. The
genetics of depression: a review. Biol Psychiatry. 2006;60(2):84-92. https://doi.org/10.1016/j.biopsych.2005.08.024
![]()