Post
spinal meningitis with subdural collection: an uncommon complication after
spinal anaesthesia for caesarean section
Seng Wee Cheo 1,*,
Qin Jian Low 2, Yee Ann Tan 3 and Yuen Kang Chia 3
1 Department
of Internal Medicine, Hospital Lahad Datu, Sabah, Malaysia.
2
Department of Internal Medicine, Hospital Sultanah Nora Ismail, Johor,
Malaysia.
3
Neurology Unit, Hospital Queen Elizabeth, Sabah, Malaysia.
*
Correspondence: cheosengwee@gmail.com;
Tel.: +6017-715-0795
Received: 26 September 2018; Accepted: 19 October 2018; Published:
24 October 2018
Edited by: Kheng Seang Lim (University of Malaya, Malaysia);
King-Hwa Ling (Universiti Putra Malaysia)
Reviewed by: Irene Looi (Hospital Seberang Jaya, Penang, Malaysia);
Tsun Haw Toh (University of Malaya, Malaysia)
https://doi.org/10.31117/neuroscirn.v1i2.18
Abstract: Meningitis after spinal anaesthesia
is a rare yet devastating complication of spinal anaesthesia. The exact
incidence is unknown. Our patient developed signs and symptoms of meningitis 48
hours after spinal anaesthesia and required intensive care unit admission. Her
cerebrospinal fluid was sterile. Computed tomography of brain showed left
subdural collection. She recovered well after 6 weeks of intravenous
antibiotics. No neurological sequela noted from subsequent follow-up
examinations. Our case provides an important insight of meningitis with
subdural collection after spinal anaesthesia for emergency caesarean section.
Keywords: meningitis; spinal anaesthesia; subdural collection;
©2018 by Cheo et al for use and distribution in accord with the
Creative Commons Attribution (CC BY-NC 4.0) license (https://creativecommons.org/licenses/by-nc/4.0/),
which permits unrestricted non-commercial use, distribution, and reproduction
in any medium, provided the original author and source are credited.
Post spinal meningitis is a rare but potentially
life-threatening complication following spinal anaesthesia. In most instances,
the presentation is typically acute, 24-48 hours after procedure. The exact
incidence is unknown. Several retrospective studies estimated the incidence to
be around 0.04%. Meningitis after spinal anaesthesia usually occurs due to
breach in aseptic technique or hematogenous spread of bacteraemia during
procedure. Here, we reported a case of post spinal meningitis with subdural
collection following spinal anaesthesia.
A 31-year-old lady, gravida 3 para 2 at 34 weeks of
gestation with twin pregnancy initially presented with labour pain.
Antenatally, this was an uneventful pregnancy. Cardiotocography (CTG) at
presentation was reactive for twin 1. CTG for twin 2 showed poor beat to beat
variation with no acceleration. She was then posted for emergency lower segment
caesarean section (LSCS) for foetal distress. She was given intravenous
ampicillin-sulbactam 1.5g as prophylactic antibiotic. Skin disinfection was
done under aseptic technique. Subarachnoid block was done at L3 level after 2
attempts. Intrathecal fentanyl 15mg and
1.9ml of bupivacaine 0.5% were given. Five minutes post spinal anaesthesia,
patient developed high spinal symptoms with sudden onset back pain and shoulder
numbness. She was resuscitated with intravenous ephedrine, phenylephedrine and
fluid. The patient subsequently responded and managed to go through the
surgery. On post operation day 2, patient complained of severe headache,
associated with neck stiffness and fever. There was no cough, no diarrhoea, no
vomiting or dysuria. Her level of consciousness was normal. Upon examination, the
blood pressure was 108/60mmHg, pulse rate was 98 beats per minute and
temperature was 40oC. Full blood count indicated haemoglobin level
was 8.6g/dl, white blood cell count was 12.9x109/L and platelet
count was 291x109/L. Renal profile was normal. Bicarbonate level was
11.9mmol/L (Table 1). She was then admitted to intensive care unit and
intubated for respiratory distress. At the same time, she was given intravenous
2g of meropenem three times a day for suspected post spinal meningitis.
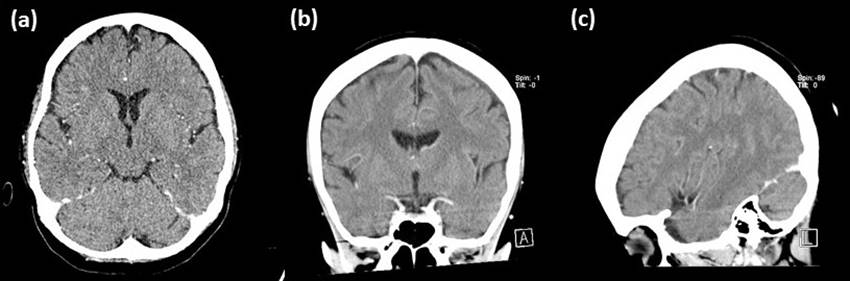
Subsequently, she undergone contrast enhanced computed tomography of the brain
which showed meningeal enhancement with left fronto-parietal subdural
collection with maximum thickness of 5mm (Figure 1). We then performed a spinal
tap on the following day. No cells were seen during CSF examination, total
protein level was 0.21g/dl and glucose ratio was normal. Both CSF cultures and
latex agglutination test were negative. She was then treated with 6 weeks of
intravenous ceftriaxone 2g twice daily. Interval CT scan of brain showed marked
improvement (Figure 2). Eventually, she recovered.
Spinal anaesthesia has been widely practised in recent
years for caesarean section [1]. Complications of spinal anaesthesia
include post dural puncture headache, arterial hypotension, local bleeding and
nerve roots injury [2]. Serious complications such as subdural
hematoma and meningitis have also been reported [3]. Post spinal meningitis is uncommon but it
is potentially devastating. Some patients even if recover will live with
neurological deficits [4]. The exact incidence of post spinal
meningitis is unknown [1]. In a retrospective study, it was
estimated to be around 0.04%.
Table 1: Investigation chart of the patient
|
Parameters
|
Results
|
Unit
|
Normal Range
|
|
Haemoglobin
|
8.6
|
g/dL
|
13-18
|
|
Total White
Blood Cell
|
12.9
|
109/L
|
4-10
|
|
Platelet
|
291
|
109/L
|
150-400
|
|
Sodium
|
129.5
|
mmol/L
|
135-145
|
|
Potassium
|
3.3
|
mmol/L
|
3.5-5
|
|
Urea
|
3.4
|
mmol/L
|
2.8-7.8
|
|
Creatinine
|
48
|
μmol/L
|
90-110
|
|
ALT
|
35
|
U/L
|
<40
|
|
Bicarbonate
|
11.9
|
mmol/L
|
22-28
|
|
Blood Culture
|
No growth
|
|
|
|
CSF AFB/Gram
stain
|
Negative
|
|
|
|
CSF Culture
|
No growth
|
|
|
|
CSF Glucose
ratio
|
0.55
|
|
|
|
CSF Protein
|
0.21
|
g/dL
|
0.15-0.45
|
|
CSF TB PCR
|
Negative
|
|
|
|
CSF
Cryptococal antigen
|
Negative
|
|
|
Our patient undergone caesarean section for foetal
distress. She complained of severe headache associated with fever and neck
stiffness post op day 2. In this clinical context, the differential diagnosis
to be considered include post dural puncture headache (PDPH), post spinal
meningitis or post spinal subdural hematoma. In our patient, PDPH is less
likely as PDPH usually does not present with high fever and neck stiffness.
PDPH patient will not appear septic.
Post spinal subdural hematoma (SDH) is another
differential diagnosis. SDH is presumed to occur due to reduced intracranial
pressure following cerebrospinal fluid (CSF) loss, causing decompression of
brain leading to rupture of fragile bridging veins [5]. In our patient, the point against this diagnosis
is the measured Hounsfield Unit is not suggestive of hematoma and SDH usually
does not present with sepsis syndrome.

Figure 1: Pre-treatment computed tomography showing
left subdural collection. (a) axial view, (b) coronal view and (c)
sagittal view.
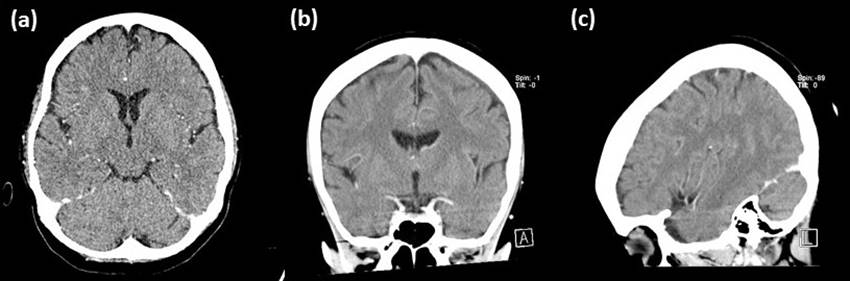
Figure 2: Interval computed tomography 2 weeks after treatment showing marked
improvement of left subdural collection. (a) axial view, (b)
coronal view and (c) sagittal view.
We think our patient had post spinal meningitis with
subdural collection because she presented with sepsis syndrome post operatively
that required ICU admission. Computed tomography of brain supported the
diagnosis of subdural collection and she responded well to antibiotic therapy.
Her CSF appeared sterile probably due to prior administration of antibiotic a
day before the lumbar puncture.
Post spinal meningitis can be broadly divided into
chemical or infective in origin [6]. The differentiation is difficult, and its
aetiology is still very much debatable. Failure of aseptic technique could
result in introduction of exogenous organisms into the cerebrospinal fluid.
Besides, hematogenous spread of infection with micro bleeding during spinal
anaesthesia could be another possibility. In bacteraemia patient, dural
puncture may facilitate entrance of bacteria into CSF [7]. Droplets infection could be another
possible route of infection [8]. Commensals of oral and respiratory tract
such as Strepcoccus spp are the frequent causative organism in post
spinal meningitis [9].
Post spinal meningitis should be suspected in patients
with spinal headache, convulsions, high grade fever and altered sensorium [10]. Other clinical features include nuchal
rigidity, coma, neurological deficits and photophobia. Blood culture and CSF
examination is mandatory if such diagnosis was suspected [11]. Brain imaging must be done to look for
complication of meningitis such as hydrocephalus or subdural collection such as
in the reported patient.
The treatment of post spinal meningitis does not
differ much from the typical treatment for meningitis. It includes early
empirical broad-spectrum antibiotics [12] and subsequent de-escalation based on
cultures and sensitivity profile. A longer treatment is needed for complicated
infection. In our patient, she was treated with 6 weeks of intravenous
antibiotics in view of the presence of subdural collection.
For prevention of post spinal meningitis, strict
aseptic technique during procedure is warranted to reduce such incidence.
Surgical mask should be worn during administration of regional anaesthesia [13]. In addition, other important aseptic
techniques such as preprocedural handwashing with antiseptic solution,
application of skin disinfectant, maintenance of sterile field and proper
sterile draping technique must be observed [14]. Local authorities should also raise the
awareness of strict adherence to aseptic technique among health care providers.
Our case illustrated a rare complication of spinal
anaesthesia which can be potentially life-threatening. It is therefore pivotal
for clinicians to properly evaluate patient with fever and headache post spinal
anaesthesia. Early treatment is important for treatment of meningitis. Full
aseptic technique is essential while performing the procedure to prevent the
occurrence of meningitis.
Consents: Written informed consent was obtained from the patient prior to
publish the case. A copy of the written consent is available for review by the
Editor-in-Chief of the journal.
Acknowledgements: The authors would like to thank the Director General
of Health Malaysia for approval to publish this paper.
Author Contributions: S.W.C., Q.J.L. and Y.A.T. drafted the paper. Y.K.C.
critically revised the article.
Conflicts of Interest: The authors declare no conflict of interest.
References
1.
Hashemi R, Okazi A. Iatrogenic meningitis
after spinal anesthesia. Acta Medica Iranica. 2008;46(5):434-436.
2.
Lambert DH.
Complications of spinal anesthesia. Int Anesthesiol Clin. 1989;27(1):51-55.
3.
Schweiger V, Zanconato
G, Lonati G, Baggio S, Gottin L, Polati E. Intracranial subdural hematoma after
spinal anesthesia for cesarean section. Case Rep Obstet Gynecol.
2013;2013:253408. https://doi.org/10.1155/2013/253408
4.
Burke D, Wildsmith JA.
Meningitis after spinal anaesthesia. Br J Anaesth. 1997;78(6):635-636. https://www.ncbi.nlm.nih.gov/pubmed/9215011
5.
Srivastava U, Agrawal
A, Gupta A, Dwivedi Y. Intracranial subdural hematoma after spinal anesthesia for
cesarean section: Case report and review of literature. advbioresnet.
2014;4(1):45-47. https://doi.org/10.4103/2249-4472.132826
6.
Lee JJ, Parry H.
Bacterial meningitis following spinal anaesthesia for caesarean section. Br
J Anaesth. 1991;66(3):383-386. https://www.ncbi.nlm.nih.gov/pubmed/2015156
7.
Singh J, Kazal S,
Kapoor D. Bupivacaine induced aseptic meningitis following subarachnoid block. Anaesth
Pain & Intensive Care. 2015;19(1):65-67.
8.
Govardhane BT,
Jambotkar TC, Magar JS. Meningitis following spinal anesthesia. Med J DY
Patil Univ. 2015;8:513-514. https://doi.org/10.4103/0975-2870.160818
9.
Gherardi S, Sher S,
Monzani R. Case Report: A Case of Meningitis of Undetermined Origin Following
Spinal Anaesthesia. Ambul Surg. 2008;14(3):60-61.
10.
Videira R, Ruiz-Neto PP,
Brandao Neto M. Post spinal meningitis and asepsis. Acta Anaesthesiol Scand.
2002;46(6):639-646. https://doi.org/10.1034/j.1399-6576.2002.460602.x
11.
Baer ET. Post-dural
puncture bacterial meningitis. Anesthesiology. 2006;105(2):381-393. https://www.ncbi.nlm.nih.gov/pubmed/16871073
12.
Doghmi N, Meskine A,
Benakroute A, Bensghir M, Baite A, Haimeur C. Aseptic meningitis following a
bupivacaine spinal anesthesia. Pan Afr Med J. 2017;27:192. https://doi.org/10.11604/pamj.2017.27.192.9327
13.
Hebl JR. The importance
and implications of aseptic techniques during regional anesthesia. Reg
Anesth Pain Med. 2006;31(4):311-323. https://doi.org/10.1016/j.rapm.2006.04.004
14. Fijter S, DiOrio M, Carmean J, Schaffzin J.
Bacterial meningitis after intrapartum spinal anesthesia-New York and Ohio,
2008-2009. MMWR Morb Mortal Wkly Rep. 2010;59(3):65-69. https://www.ncbi.nlm.nih.gov/pubmed/20110933
![]()